Iliotibial Band Syndrome (IT Band Pain) Treatment in Whitby
Iliotibial Band Syndrome (ITBS) is one of the most common causes of outer‑knee pain in runners, walkers, and cyclists. It occurs when the iliotibial band becomes irritated as it rubs over the outer knee or, in some cases, higher up near the hip. Foot instability, hip weakness, and training errors all contribute to this condition. We assess and treat IT Band pain at our Whitby clinic to reduce irritation, improve biomechanics, and help you return to activity comfortably.
What Is Iliotibial Band Friction Syndrome?
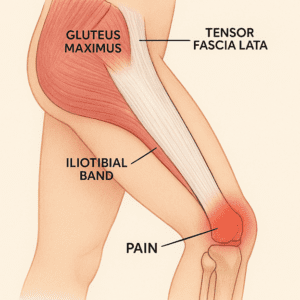
The iliotibial band (ITB) is a thickened strip of fascia running along the outside of the thigh. It originates near the anterior superior iliac spine and inserts into Gerdy’s tubercle on the tibia. It blends with the tensor fascia lata, gluteus medius, gluteus maximus, and vastus lateralis muscles. When the ITB becomes irritated—usually from repetitive bending and straightening of the knee—it can cause sharp or aching pain on the outer knee or lateral thigh.
How Foot Instability Contributes to IT Band Pain
Foot mechanics play a major role in ITB irritation. When the foot collapses inward (excessive pronation), the tibia rotates medially, increasing tension on the ITB. Over time, this repetitive strain leads to inflammation and pain. Stabilizing the foot can reduce knee rotation and decrease stress on the ITB.
Common Causes of IT Band Syndrome
Biomechanical Factors
- Weak hip abductors
- Muscle imbalance between gluteal and thigh muscles
- Excessive foot pronation
- Tight iliotibial band or tensor fascia lata
Training Errors
- Sudden increase in running mileage
- Increased interval or track training
- Running on crowned or uneven surfaces
- Overstriding or long stride length
Symptoms of IT Band Friction Syndrome
-
Sharp or burning pain on the outer knee
-
Pain that worsens with running, especially downhill
-
Tenderness along the lateral thigh
-
Possible hip discomfort if the upper ITB is irritated
Evidence‑Based Treatment Options
ITBS often requires a combination of activity modification, strengthening, and biomechanical correction.
Activity Modification
- Reduce or temporarily stop running
- Avoid crowned roads and repetitive track running
- Shorten stride length to reduce ITB tension
Strengthening & Stretching
- Strengthen hip abductors (focus on gluteus medius)
- Stretch the ITB, TFL, and gluteal muscles
- Use overhead arm extension to improve ITB lengthening
Footwear & Orthotics
- Motion‑control shoes to limit excessive pronation
- If already in motion‑control shoes, consider switching to a less controlling model
- Custom foot orthotics to stabilize foot mechanics and reduce knee rotation
Clinical Interventions
- Manual therapy
- Laser therapy
- Corticosteroid injection for persistent inflammation
- Surgical release (rare; reserved for chronic, non‑responsive cases)
When IT Band Pain Doesn’t Improve
If symptoms persist despite proper stretching and strengthening, another condition may be mimicking ITBS. Differential diagnoses include:
-
Lateral meniscal tear
-
Lateral collateral ligament sprain
-
Biceps femoris tendinopathy
-
Patellofemoral pain syndrome
-
Lateral patellar compression
-
Popliteal tendinopathy
-
Stress reaction or stress fracture
-
Proximal tib‑fib joint sprain
-
Referred pain from lumbar spine or peroneal nerve
When to Seek Professional Assessment
Persistent lateral knee or thigh pain should be evaluated by a chiropodist. A biomechanical exam, gait analysis, and footwear assessment help identify the root cause and guide treatment.
IT Band Pain Treatment in Whitby
We assess foot posture, hip strength, gait mechanics, and training patterns to determine why your ITB is irritated. Treatment focuses on reducing tension, improving alignment, and restoring comfortable movement.
Book an Appointment
Book an appointment If you’re experiencing IT Band pain, early assessment helps prevent chronic irritation and speeds recovery.
References
- Conservative Rehabilitation Treatments of Iliotibial Band Syndrome: A Systematic Review. Muscles, Ligaments and Tendons Journal. 2021;11(1):29-40.
- Effects of conservative treatment strategies for iliotibial band syndrome on pain and function in runners: a systematic review. Frontiers in Sports and Active Living. 2024;6:1386456.
- Gender Differences in the Kinetics and Kinematics of Distance Running: Implications for Footwear Design. International Journal of Sports Science and Engineering. 2012;6(2):118-128.
- The Influence of a Prefabricated Foot Orthosis on Lower Extremity Mechanics During Running in Individuals With Varying Dynamic Foot Motion. JOSPT. 2016;46(9):749.
- Iliotibial Band Impingement Syndrome: An Evidence-Informed Clinical Paradigm Change. International Journal of Athletic Therapy & Training. 2017;22(3):1-11.
- The Top Five Running Injuries Seen in the Office. Podiatry Management. 2013; April & June issues.
