Patello‑Femoral Pain Syndrome (PFPS) Treatment in Whitby
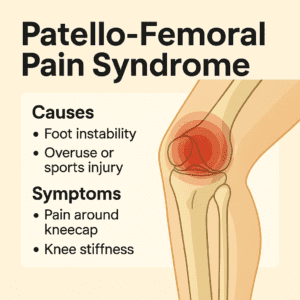
PFPS occurs when the kneecap (patella) does not track smoothly in its groove, leading to pain around or behind the knee. It’s one of the most common running‑related injuries, especially in women and adolescents. At Whitby Family Footcare Clinic, we assess foot posture, gait mechanics, and muscle balance to reduce pain, improve alignment, and restore comfortable movement.
What Is PFPS?
The patella sits within a tendon that crosses the front of the knee. As the knee bends, the patella glides in a groove on the femur. When alignment is disrupted often due to foot instability, muscle imbalance, or biomechanics the patella may shift laterally, increasing pressure and irritation.
PFPS accounts for nearly 1 in 4 running injuries and is often aggravated by walking, running, stair climbing, or prolonged sitting.
Common Symptoms of PFPS
-
Dull ache around or behind the kneecap
-
Pain during running, jumping, or stair climbing
-
Discomfort when sitting with knees bent (“theater sign”)
-
Knee stiffness or swelling
-
Cracking or popping sounds
-
Quadriceps weakness or the knee “giving out”
Why PFPS Happens: Anatomy & Biomechanics
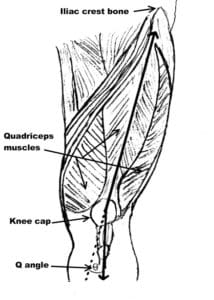
PFPS develops when the quadriceps and patella are not working in balance:
-
The quadriceps originate at the pelvis and attach to the patella.
-
The patellar ligament connects the patella to the tibia.
-
The patella acts like a pulley, improving knee extension efficiency.
If the vastus medialis is weak or surrounding tissues are tight, the patella may drift laterally, increasing joint stress and pain.
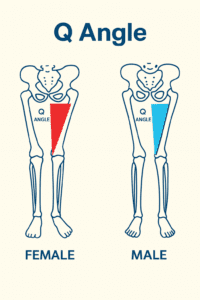
The Role of Q Angle
The Q angle is formed between:
-
A line from the front of the hip (ASIS) to the center of the patella
-
A line from the patella to the tibial tubercle
A larger Q angle—common in females due to wider hips—can cause lateral patellar tracking. Excessive foot pronation increases this angle, adding stress to the knee.
How Foot Instability Contributes to PFPS
Unstable foot posture alters leg alignment during walking and running. When the foot rolls inward excessively:
-
The tibia rotates
-
The patella is pulled laterally
-
Pressure beneath the kneecap increases
This chain reaction contributes directly to PFPS symptoms.
Contributing Factors
PFPS often results from a combination of:
-
Poor foot posture
-
Unstable or worn‑out footwear
-
High training intensity
-
Occupational demands
-
Anatomical variations around the knee
Treatment Options
PFPS is typically managed without surgery. Effective strategies include:
- Rest and activity modification to reduce irritation
- Ice therapy to manage inflammation
- Anti‑inflammatory medications (general information only)
- Physiotherapy and strengthening to improve quadriceps balance
- Stretching and massage for tight tissues
- Knee taping or bracing to support patellar tracking
- Custom foot orthotics to correct foot posture and reduce knee stress
- Supportive footwear to improve alignment
If symptoms persist, referral to physiotherapy, sports medicine, or orthopedics may be recommended.
When to Seek Care
Assessment is recommended if you experience:
- Persistent pain beneath or around the kneecap
- Difficulty with stairs, running, or prolonged sitting
- Recurrent swelling or stiffness
- A feeling of instability or the knee “giving out”
PFPS Treatment in Whitby
We assess:
-
Foot posture and gait mechanics
-
Quadriceps strength and patellar tracking
-
Footwear and activity demands
Our goal is to reduce pain, improve alignment, and restore confident movement.
References
- Global research trends and hotspots in patellofemoral pain syndrome from 2000 to 2023: a bibliometric and visualization study. Frontiers in Medicine. 2024.
- Effect of physiotherapy interventions on pain management, function and quality of life in patellofemoral pain syndrome: A systematic review protocol. PLOS One.
- Effects of functional strength training on pain, function, and lower extremity biomechanics in patients with patellofemoral pain syndrome: a randomized clinical trial. Journal of Orthopaedic Surgery and Research. 2025.
- The immediate effects of foot orthoses on functional performance in individuals with patellofemoral pain syndrome. British Journal of Sports Medicine. 2011;45(3):193–197.
